Accurate wound assessment is essential when determining the treatment plan for a wound. And yet, studies have repeatedly demonstrated the unreliability of clinical signs and symptoms for detecting wounds with uncontrolled bacterial burden and infection.1,2 Gold-standard microbiological confirmation to determine bacterial presence delays treatment by at least 24 hours and is prone to sampling errors. Use of the MolecuLight i:X to image for bacterial fluorescence, in conjunction with clinical signs and symptoms, adds an additional, bacterial-specific piece of information that can be captured and considered at the patient’s bedside prior to prescribing a treatment plan.

Clinician's Testimonial
"My standard wound assessment revealed no signs and symptoms of infection. But the fluorescence images taken with my MolecuLight i:X told a different story. It was the images that led to this patient receiving the in-patient and antibiotic care that she required."
Rosemary Hill, BSN, CWOCN, CETN(C), Vancouver Coastal Health, Vancouver, BC, Canada
Clinician Profile
Rosemary Hill, BSN, CWOCN, CETN(C), with over 12 years of wound care experience, oversees wound care for inpatients and outpatients at Lions Gate Hospital, Vancouver Coastal Health, located in North Vancouver, Canada. Rosemary is a past President of the Canadian Association for Enterostomal Therapy (CAET).
Clinical Synopsis
Patient Condition: 63-year-old lymphoma patient’s large, untreated sacral pressure injury was discovered by the outpatient chemotherapy unit.
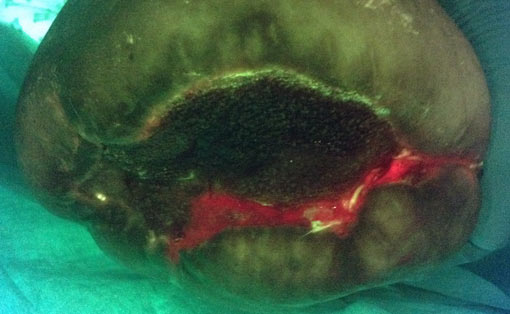
During a routine outpatient chemotherapy appointment, this lymphoma patient mentioned in passing a “large blister” that had developed on her bottom. This turned out to be a large, untreated sacral pressure injury (6 cm x 6 cm, 100% slough) and the hospital wound care specialist was called in for a thorough assessment. Standard assessment based on clinical signs and symptoms of infection did not suggest infection in this wound. However, the wound care clinician proceeded to image the patient’s wound with the MolecuLight i:X, which showed extensive bioburden (red fluorescence) within and around the wound bed (Figure 2), resulting in immediate hospital admission for treatment including systemic antibiotics. Swabs taken from these regions of red fluorescence were later confirmed to be heavy growth of Staphylococcus aureus and Escherichia coli. Throughout treatment, the MolecuLight i:X was also used to guide debridement of this patient’s wound, targeting areas of red fluorescence and sparing healthy tissues.
After 7 days of antibiotic treatment and negative pressure wound therapy (NPWT), bacterial fluorescence in the wound bed was notably decreased (Figure 4). Hospital-based wound care treatment continued for 2 months before transferring the patient to a residential care setting. Six months after discovering the wound, it had decreased in size to 2 cm x 1.3 cm x 1.5 cm with 100% granulation tissue.
 |
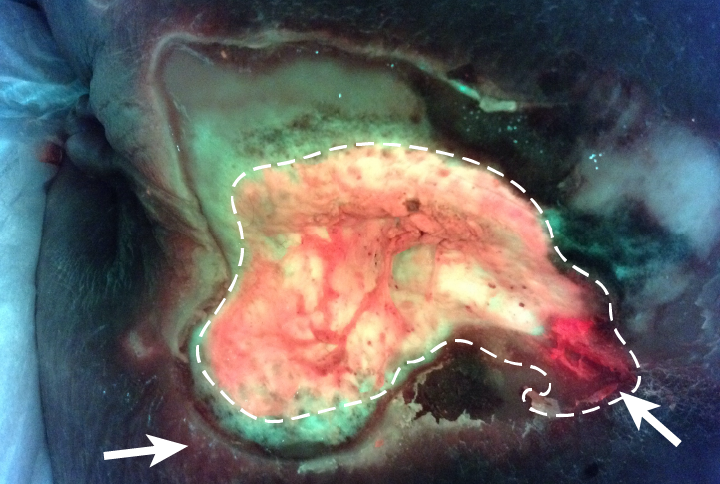 Bacteria appear red/blush pink in image |
|
 |
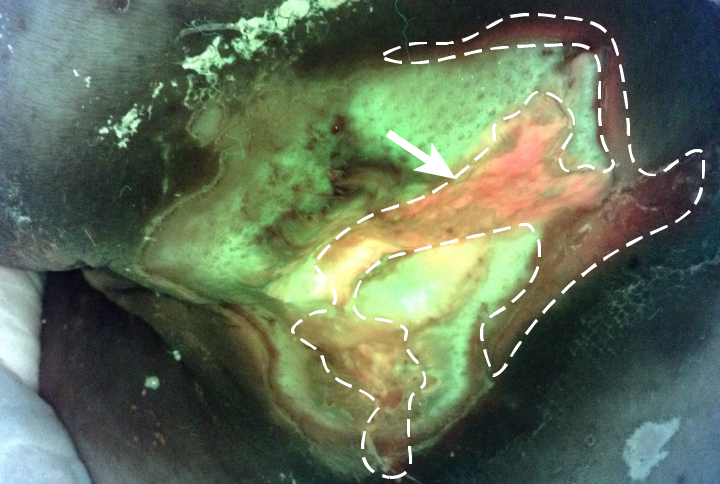 Bacteria appear red/blush pink in image |
At a glance
| Wound etiology & location | Pressure ulcer, sacrum (6 cm x 6 cm, 100% slough) |
| Patient demographics | Female, 63 years old |
| Patient-related challenges | Lymphoma
Type II diabetes and diabetic retinopathy Hypertension and dyslipidemia Hypothyroidism |
| Patient’s general care paradigm | Systemic antibiotics
Targeted debridement and NPWT |
| Confirmed microbiology results | Swabs taken from regions of red fluorescence confirmed heavy growth of Staphylococcus aureus and Escherichia coli |
| Clinician stated utility of the MolecuLight i:X | Identification of uncontrolled, asymptomatic bacterial burden requiring hospitalization and antibiotic therapy
Guided debridement Guided sampling |