ABSTRACT
Aim:
Wound surface area reduction is used as a predictor of healability and an indication of the care protocol efficacy. The variability, of up to 40%, in standard length x width estimation of wound surface area is unacceptable on a measurement on which care decisions are being based. Digital planimetry tools have been demonstrated to be more accurate and consistent than conventional methods in documenting the progress of a wound through the care continuum. Here we present the use of a hand-held, non-contact wound imaging device that includes fluorescence imaging and documentation of bacteria and software that estimates and documents the area of a wound, using a proprietary algorithm or manual trace functionality.
Method:
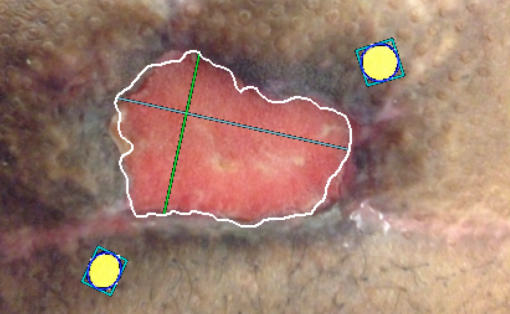
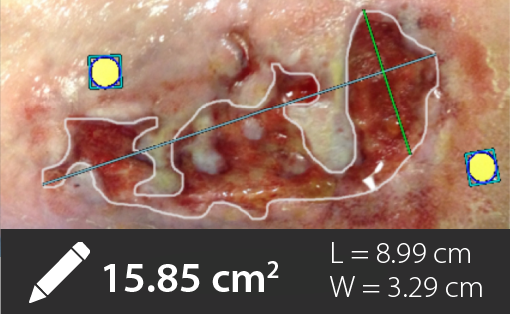
25 wounds were imaged for up to 8 weeks and their progress was documented with fluorescence images of bacterial location and surface area measurements, using either the automatic trace feature or the manual trace feature.
Results/Discussion:
All wound measurements were over estimated by conventional methods, with a maximum error of 50%. 10% of wounds areas were estimated using the auto-trace functionality, whereas 90% of the wounds areas were better estimated by manual trace of the wound border. 14/25 wounds had surface area reduction indicative of a healing trajectory (30% in 4 weeks), whereas 11/25 wounds were stalled and candidates for care protocol re-assessment.
Conclusion:
Accurate and convenient wound area measurement in a point-of-care, hand-held imaging device is helpful in documenting wounds and predicting their healability in an objective, standardized manner.